A 58 year old male, labourer,came to the OPD with chief complaints of SOB since 12 days, It got worsened 2 days back, puffiness of the face since 1 week.
A 58 year old male, labourer,came to the OPD with chief complaints of SOB since 15 days, worsened 3 days back, facial puffiness since 1 week
History of Presenting illness -
Patient was apparently asymptomatic 4 years ago.
4 years ago - pt complained of giddiness, went to a local hospital and was diagnosed as Hypertensive, on regular medication since then T. Nicardia 10mg, T. Arkamine 0.1mg sos.
2 years back Pt developed B/L pedal edema, progressed gradually to knees, diagnosed with renal failure and initiated dialysis weekly twice.
Left upper limb swelling, gradually progressing to current size, since 4 months . Swelling in the left chest region, gradually progressing to current size, since 4 months
Back pain since 2 months, subsided on medication .
7 days back - developed Facial puffiness
Shortness of breath since 7days.
Grade II-III progressed to Grade IV since 15 days along with orthopnea .
No c/o palpitations, giddiness, cold, cough, burning micturition
PAST HISTORY -
K/c/o Hypertension since 4years on Tab nifedipine 10mg OD
Not K/C/O TB, Epilepsy, Asthma, CAD.
Personal history
Appetite- normal
Diet- mixed
Bowel movement- Regular
Alcoholic stopped 4 yrs ago
Non smoker
On examination
Pt is conscious, coherent and cooperative.
Pallor - absent
Icterus - absent
Cyanosis - absent
Lymphadenopathy - absent
Edema of feet - present
VITALS :
Pulse :94bpm
Bp:120/80
Spo2:97% at RA
Temp - Afebrile
Systemic Examination:
CVS - S1,S2 +
RS - BAE +
CNS - NAD
P/A- Soft, non tender
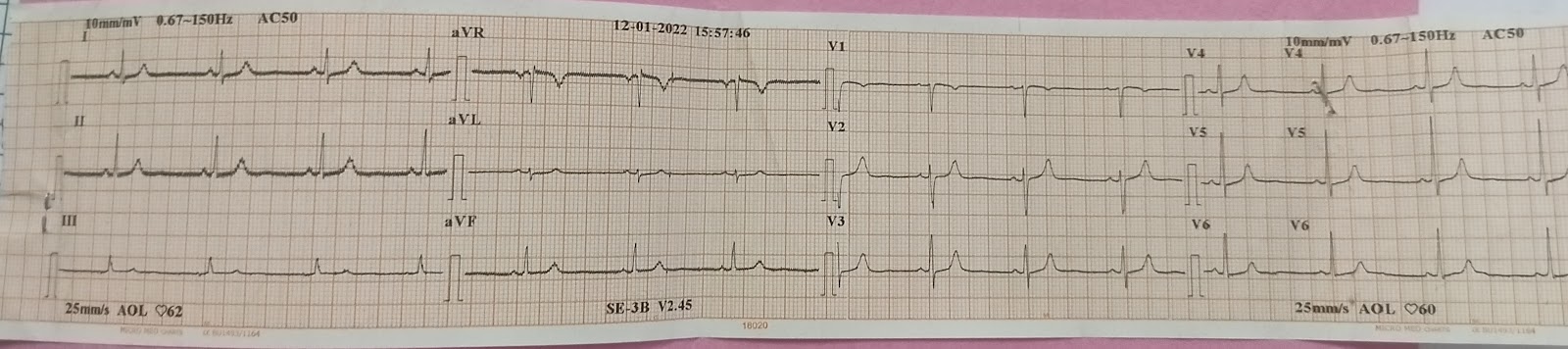
INVESTIGATIONS
Serology - Negative
PROVISIONAL DIAGNOSIS -CKD on Maintenance Hemodialysis.
Treatment-
Fluid restriction (<1l/day)
Salt restriction (<2g/day)
T· LASIX 40 mg PO BD
T. Nicardia 100mg PO BD
T. NODOSIS 500 MG PO BD
T. OROFER-XR PO OD
T. SHELCAL-CT PO OD
CLINICAL IMAGES